At the age of 11, Kerry Esrey, a second-year English student, was diagnosed with Type 1 diabetes.
“I had to get used to a new way of living. Every time I ate, I had to think about it, and I couldn’t eat whenever I wanted to and had (stress) from having to check (and correct) high and low blood sugars,” Esrey said.
Among the new changes Esrey had to adapt to were testing her blood sugar regularly and adjusting insulin levels accordingly. Despite these changes in her routine, Esrey said that her social and familial life remained constant because she had everyone’s support.
“Having diabetes is a full-time job,” said Shiri Morgan, registered dietician and diabetes educator at the Gonda Goldschmied Diabetes Center. It is key to learn how to control diabetes by gaining a thorough understanding of the course of action to follow and its importance.
The Gonda Goldschmied Diabetes Center at UCLA focuses on research to improve understanding of diabetes and treatments while catering to patient needs and teaching them how to take care of themselves, said Dr. Peter Butler, professor of medicine, and director of Larry L. Hillblom Islet Research Center.
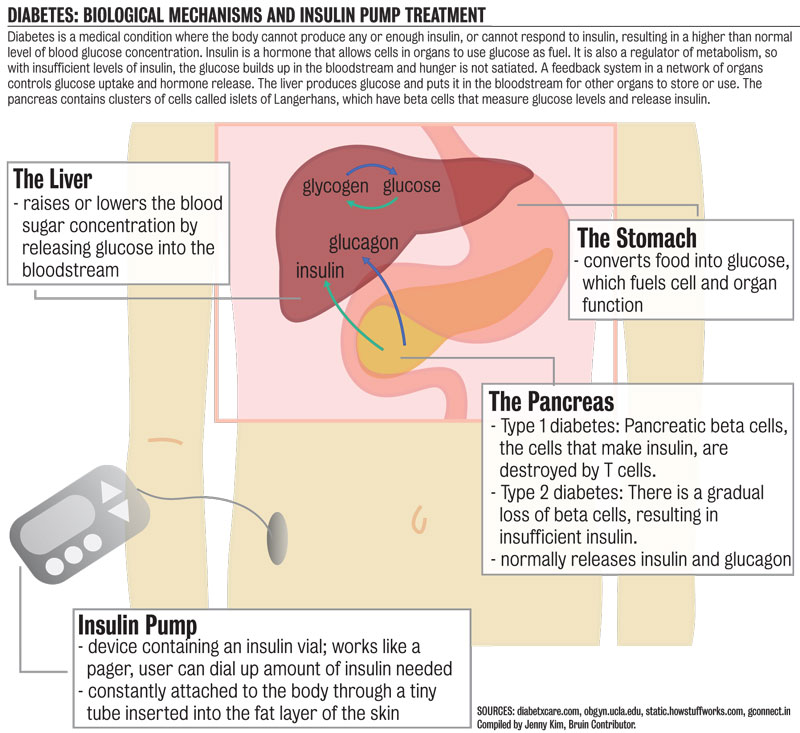
Diabetes occurs when blood sugar concentration levels exceed the norm. Usually, a complex network of different organs regulates blood sugar levels, Butler said.
One of these organs is the liver, which makes sugar and puts it in the blood while other organs such as muscle tissue store it and use it as fuel for energy demands.
The other organ is the pancreas, and within the pancreas, there are islets of langerhans. These include a special kind of cell called beta cells, which measure the levels of blood sugar and work with the liver to establish normal blood sugar.
More than 250 research papers have been published in UCLA on studies about diabetes, Butler said. One of UCLA’s important breakthroughs included the center showing that Type 1 diabetes continued to make new pancreatic beta cells. Another research product was the discovery that the deficit of pancreatic beta cells was due to their high death rate in Type 2 diabetes.
Research for Type 1 diabetes is focused on cell therapy, the ways of making new kinds of cells that would act like pancreatic beta cells, therefore replacing insulin injections.
Efforts for Type 2 have focused on increasing the understanding of why the cells in the langerhans islets get killed and if there are ways to improve the amounts of cells left alive.
There exist two major kinds of diabetes, both of which are related to the number of beta cells that live in the islets of langerhans within the pancreas. In Type 1 diabetes, the body’s defense system produces T cells to fight the virus. There is a body error that causes these cells to recognize pancreatic beta cells as foreign, therefore destroying them. This results in a need for insulin injections to balance the blood sugar levels.
Type 2 diabetes is the product of a gradual loss of cells that make insulin, resulting in insufficient insulin. Its causes include being overweight and/or obese and undergoing sleep disturbance, making college students prone to it, Butler said.
Commercial efforts to manufacture alternative method of insulin injection have manufactured the pump, Butler said.
When Esrey was first diagnosed, she had to take injections about three times a day. Six months after her diagnosis, she went on the insulin pump, a device that consists of an insulin vial outside of the body with a pager-like dial, and a tiny tube inside the fat of the body, Esrey said.
“(The insulin pump) made it more practical because I’m always on the go. It’s a way for me to have more freedom,” Esrey said.
In order to help its patients control their diabetes, the Gonda Center, a multi-disciplinary program, offers its patient either one-on-one counseling or education groups, Morgan said.
Within the classes, three components are identified to help manage diabetes; diet, exercise and medication, Morgan said.
“We are trying to develop other classes for people using the pump, for pregnant diabetics, and (designed for) preconception care,” Morgan said.
Esrey has created a group for UCLA diabetics to gather and discuss their disease as well as form a community, she said.
Esrey and the 10 other students in the group hope to participate in the Walk to Cure Diabetes next year and grow in size over the course of the next few years.
“Luckily, I’ve been keeping a positive attitude about diabetes; you can pretend you don’t have it and develop complications in the future, or say “˜Hey, I have it,’ and learn to deal with it,” Esrey said.