A team of UCLA-led researchers has identified a new natural antiviral compound that may be able to reduce the effects of deadly human viruses, such as HIV.
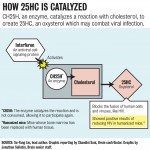
In a study conducted by researchers from UCLA and other universities, the research team discovered that a compound called 25-Hydroxycholesterol, which is a cholesterol derivative and is classified as an oxysterol, has antiviral properties. Oxysterols have various biological functions, including helping keep cholesterol molecules stable.
This oxysterol is formed when interferon, an antiviral signaling protein in the body, triggers the immune system and activates an enzyme referred to as CH25H, said Su-Yang Liu, the lead author of the study and a third-year medical student. The enzyme converts cholesterol into 25HC, which then blocks the fusion of human and virus cells, preventing the virus from infecting the human cell.
Liu and the other researchers discovered the enzymatic reaction’s antiviral potential in 2009 and have been doing testing ever since. Results from the study, which was funded by National Institutes of Health grants, Student Training and Research in Tumor Immunology Grant and the Warsaw Fellowship, were completed recently and published in the January edition of the scientific journal Immunity.
While more research remains to be done, Liu said the team hopes that this study will lead to further discoveries in treatment of diseases like HIV in the long run.
“For now, the discovery of the antiviral properties of the enzyme changes the way scientists think about oxysterols,” Liu said. “I don’t want to say that we are trying to cure AIDS tomorrow.”
The researchers are not only testing oxysterol against HIV, but also against other viruses. They first tested 25HC against nine diseases including Ebola, HIV, herpes and Rift Valley fever in the lab in order to see whether it could be used to prevent those viruses, said Roghiyh Aliyari, a co-author of the study.
The researchers then moved on to animal testing. They tested the oxysterol against HIV in humanized mice, whose bone marrow system was replaced with human tissue. When researchers administered the protein to the mice, the injections greatly reduced the prevalence of HIV in the mice, Liu said. Although the protein did not fully cure the mice, it significantly reduced the number of HIV-infected cells in their systems.
Arleen Leibowitz, a professor emeritus in the department of public policy at the UCLA Luskin School of Public Affairs whose area of expertise is HIV/AIDS, said there are many other factors to consider in HIV treatment even if the recent discovery was a potential antidote.
She said she is hesitant about using the word “cure” regarding 25HC and its effects on HIV.
“We would have to figure out how to produce enough of it to treat everyone in the United States who has HIV and how to pay for it,” Leibowitz said. “One would have to see what the cost relative to the current retroviral is and whether it is safe in the long run.”
There are also some short-term problems that the researchers will have to address in terms of the shortcomings of the research. Some potential weaknesses include that 25HC is difficult to administer in large doses and that the researchers have yet to do animal testing for diseases besides HIV, according to a press release from the UCLA Health System.
Liu said he recognized how much work still has to be done. The researchers hope that the compound can be used to treat diseases including AIDS in the future, but think that the immediate implication is that it will change their idea of how oxysterols work, Liu said.
Liu added that the researchers hope other artificial oxysterols with better antiviral properties can be produced in a lab to combat viruses in human cells.